

What is BPH?
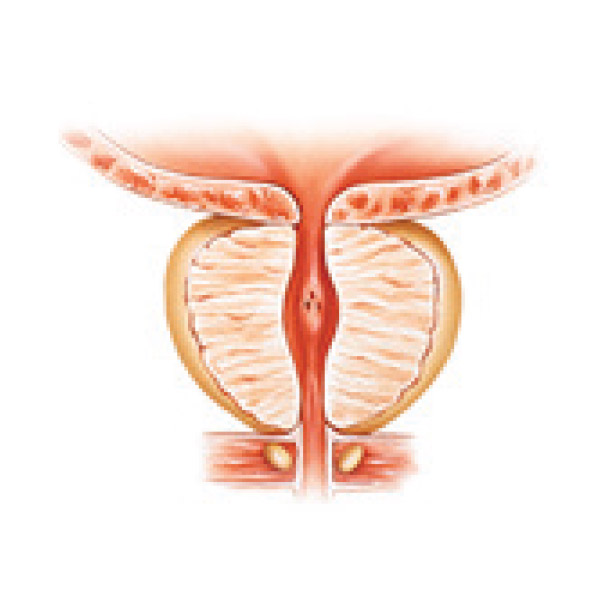
The prostate is a small gland located right below the neck of the bladder and is part of the male reproductive system. The urethra, which carries urine from the bladder outside the body, runs through the prostate gland. Prostatic fluid is a component of semen and plays a role in expelling semen during ejaculation.
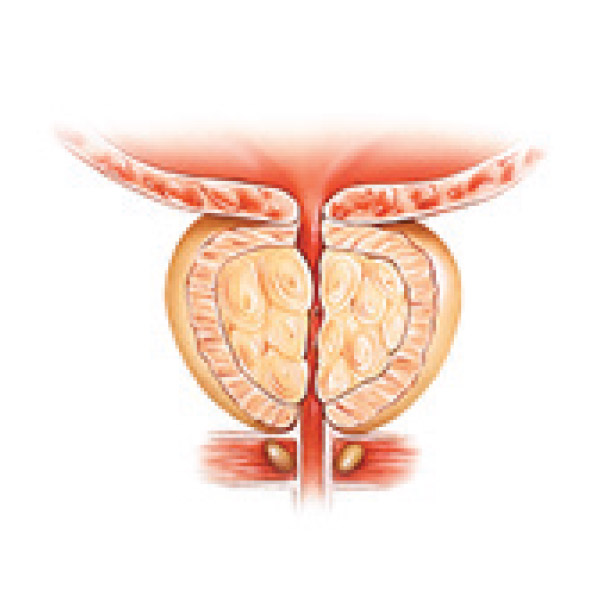
A healthy prostate gland is approximately the shape and size of a walnut. As men age, the prostate gland often becomes enlarged. This very common process is called Benign Prostatic Hyperplasia (BPH), or enlarged prostate. This causes the prostate to press against the urethra, causing chronic and troublesome lower urinary tract symptoms that can severely affect your quality of life. These include:
- difficult urination
- frequent need to urinate
- weak stream
- difficulty to start urination
- not being able to sleep through the night
- difficulty in voiding completely
- leakage
- sexual dysfunction
- and more.
This non-cancerous growth of the prostate affects over 500 million men worldwide and is one of the leading reasons men visit a urologist.


Do I have BPH?
The American Urological Association (AUA) has created a symptom index to help you and your physician understand and measure the severity of your symptoms. While only your doctor can make a diagnosis, this quiz can help you toward seeking proper care.
Mark your responses below, click SUBMIT to receive your total score, and bring this to your doctor to discuss your options.
Treatments for BPH
If you have been diagnosed with an enlarged prostate due to BPH, it is important to be monitored by a urologist. If left untreated, BPH can affect erectile function and libido, and can lead to urinary tract infections (UTI), stones in the bladder or kidney, urinaryretention and kidney damage.
The good news is that there are many treatment options available. Ask your doctor which one is right for you.
Wait & Watch
If your symptoms are mild and do not affect your quality of life to a great degree, your doctor may recommend a conservative “wait and watch” approach. Together you and your doctor will monitor your condition by tracking your symptoms.
Medication
There are a number of prescription medications to manage BPH symptoms. These include alpha blockers, which relax the muscles around the neck of the bladder making it easier to urinate. Alpha reductase inhibitors are used to shrink the prostate. While medications often offer symptom relief, the downside is that you must continue taking them over the long-term to maintain this relief. And unfortunately, these medications have also been reported to cause troubling side effects. These include dizziness, headaches, and sexual dysfunction.
iTind Treatment
The iTind (Temporarily Implanted Nitinol Device) treatment is a minimally invasive, 5-day treatment introducing a completely new and different approach. The treatment gently reshapes the urethra, creating new channels for urine to flow. There are none of the side effects associated with prescription medications, and none of the risks to sexual function and urinary continence which can occur with major surgery. And unlike other non-surgical BPH procedures, the iTind involves no heating or removal of prostate tissue, and no permanent implant is left behind.
Permanent Implants
There are a number of permanent metal implants that are designed to mechanically hold prostate tissue back from the urethra to ease the flow of urine. Most permanent implants are placed via a minimally invasive procedure that allows relatively rapid recovery time. However, reliance on a permanent implant in the prostate carries certain risks, such as migration to other areas of the body or becoming encrusted which can lead to bladder stones. If this happens or symptoms recur, they must be surgically removed or cut out of the tissue.
Heat Therapies
Minimally invasive thermotherapies apply heat energy, like radio frequency (RF), microwave or steam to the prostate tissue to shrink it. These treatments provide moderate symptom relief for some patients, are generally considered safe and can be performed under local anesthesia. The risks are that applying heat to the prostate can actually cause the tissue to swell while doing its job and lead to uncomfortable urinary symptoms during the healing period. This may result in longer recovery time. Symptom relief is usually not immediate and patients recuperate with a catheter.
Laser
Laser resection of the prostate is a less-invasive surgical procedure. Known as photoselective vaporization of the prostate (PVP) or holmium laser enucleation (HOLEP), there is significantly less risk of bleeding with laser surgery versus conventional Conventional Transurethral Resection of the Prostate (TURP) surgery. Since prostate tissue is removed, there is sometimes swelling and discomfort during healing and this can lead to longer downtime and recovery. Apart from bleeding, the risks and complications are similar to those seen with TURP and typically a catheter is required after the procedure.
Conventional Transurethral Resection of the Prostate (TURP)
TURP is the most common surgery to treat BPH. This is major surgery. Patients undergo general anesthesia to remove prostate tissue. TURP is considered the “gold standard” for long-term results. Like any major surgical procedure, the body requires time to heal and recuperate. Potential risks include inflammation of the remaining prostate tissue prior to the desired reduction effect. Other side effects and complications from the surgery include bleeding, infection, urethral strictures, erectile dysfunction, retrograde ejaculation and urinary incontinence. Patients must have a catheter inserted into their bladder for several days after the procedure. While symptom relief may not be immediate, successful procedures do produce long-term symptom relief in most patients. And there is significant downtime to recuperate.


